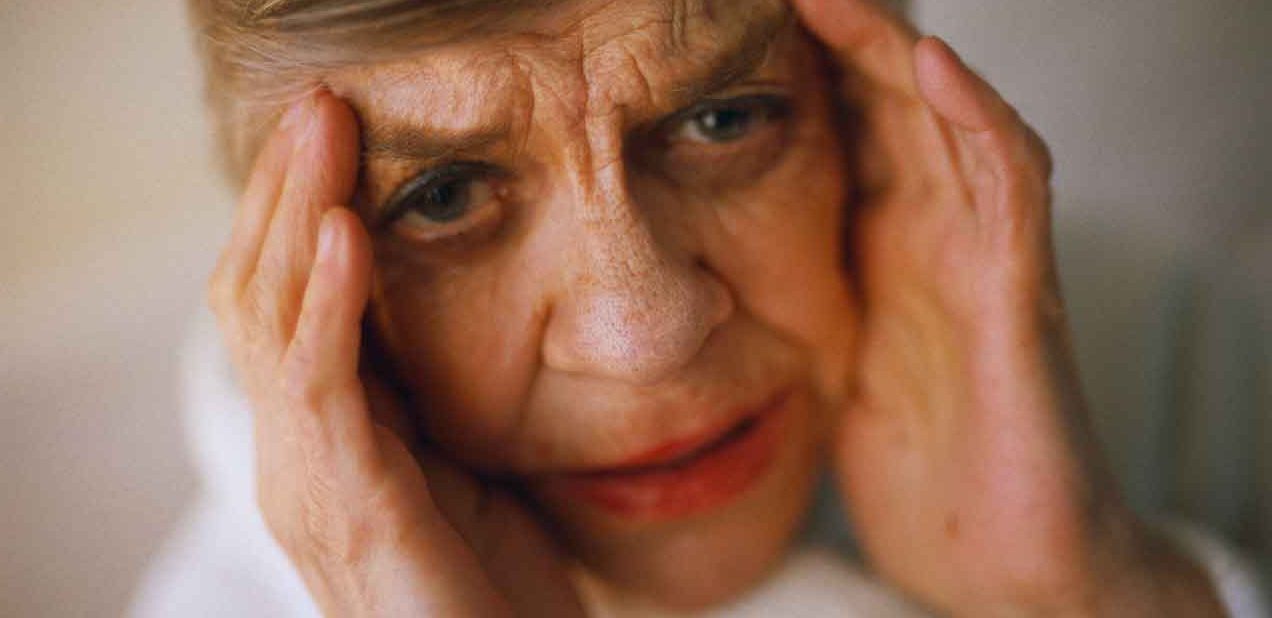
Personality Changes and Early Signs of Dementia
A new diagnosis could detect early signs of dementia and help identify patients at risk for Alzheimer’s disease and other forms of memory loss.
Alzheimer’s disease, the most common form of severe memory impairment, accounts for between 60 and 80 percent of dementia cases. It is a deadly disease that includes memory loss, anxiety, confusion, depression, and sometimes aggressive behavior. According to the Alzheimer’s Association, more than 5 million people in the United States are living with Alzheimer’s.
There is no cure. But a potential new diagnosis presented at the Alzheimer’s Association International Conference in July, could help predict whether a person is at risk for severe memory impairment or cognitive decline.
YOU MIGHT ALSO LIKE: Finally, Some Helpful News about Dementia
Dementia and mild behavioral impairment
The new diagnosis is known as mild behavioral impairment, or MBI, and it may be one of the early signs of dementia.
Mild behavioral impairment is a form of personality change that involves five types of behavior: apathy/drive/motivation, impulse control/agitation/reward, mood/affect/anxiety, thoughts/perception, and social appropriateness.
The diagnosis is based on the idea that gradual but significant changes in behavior can be one of the early signs a person is at risk for, or is already developing, dementia.
The researchers who proposed the new MBI diagnosis offered a checklist of 34 points as a tool for detection. The questions on the checklist focus on personality and behavioral changes that have occurred, such as, “Has the person lost the motivation to act on their obligations or interests?” and “Does the person display a new recklessness or lack of judgment when driving?” These changes, researchers emphasize, should not be sporadic or temporary, but need to have occurred for a period of six months or longer in order for a diagnosis of mild behavioral impairment to be given.
The questions are designed to be used by family members, caregivers, and doctors. They offer a way to track significant personality changes over time and see how a patient or loved one is progressing.
A new way to evaluate dementia
More significantly, the MBI checklist would be a change in how doctors evaluate a patient for forms of dementia like Alzheimer’s. Currently, diagnosis focuses on memory loss and cognitive impairment. But behavioral changes can be one of the earliest — and often overlooked — signs that the brain is deteriorating, according to Maria C. Carillo, the chief science officer of the Alzheimer’s Association.
“By looking beyond memory-related issues to closely evaluate the behavioral issues included in the checklist, physicians could reach a more efficient and accurate diagnosis, sooner," said Carrillo in a press release put out by the Alzheimer’s Association.
Risks and benefits of early detection
Tracking the behavioral changes that occur with MBI could help doctors identify patients who are at high risk for developing dementia. It would also provide answers to caregivers and family members who are confused by alterations in a loved one’s personality.
Many times people closest to dementia patients are the first to notice these types of early warning signs, but they aren’t aware of what they signify. Using the checklist would provide answers and allow doctors to suggest medication or lifestyle modifications that could help manage some of the symptoms.
Is the test too broad?
The type of early detection that the MBI checklist would provide is not without controversy in the medical community. Some doctors and researchers believe that diagnosing mild behavioral impairment would put patients, caregivers, and insurance companies on high alert for dementia that may never actually develop.
Kenneth Langa, MD, PhD, a professor of internal medicine at the University of Michigan, is one of the wary ones. “There’s the potential benefit of... identifying people more likely to decline,” Langa told The New York Times. “The flip side is overdiagnosis, labeling someone and getting people in the clinical cascade, where you start doing the test and people start doing more brain imaging and being at the doctor’s more and getting more concerned.”
This could be especially frustrating for some families, as there is currently no cure for Alzheimer’s and other forms of dementia.
Zahinoor Ismail, MD, one of the doctors who developed the checklist, believes that identifying instances of mild behavioral impairment could only help. By providing a new way of evaluating neuropsychiatric symptoms, or NPS, the checklist does more than just help doctors diagnose their patients. "[The checklist] is significant not only clinically, but also in research,” Ismail said in the Alzheimer Association’s press release. “From a research perspective, the scale may prove to be usable in... observational studies to help assess the impact of NPS in older adults."
Those studies could help researchers make new advances in not only treating but eventually curing dementia.
Updated:
March 05, 2020
Reviewed By:
Janet O’Dell, RN