Congestive Heart Failure
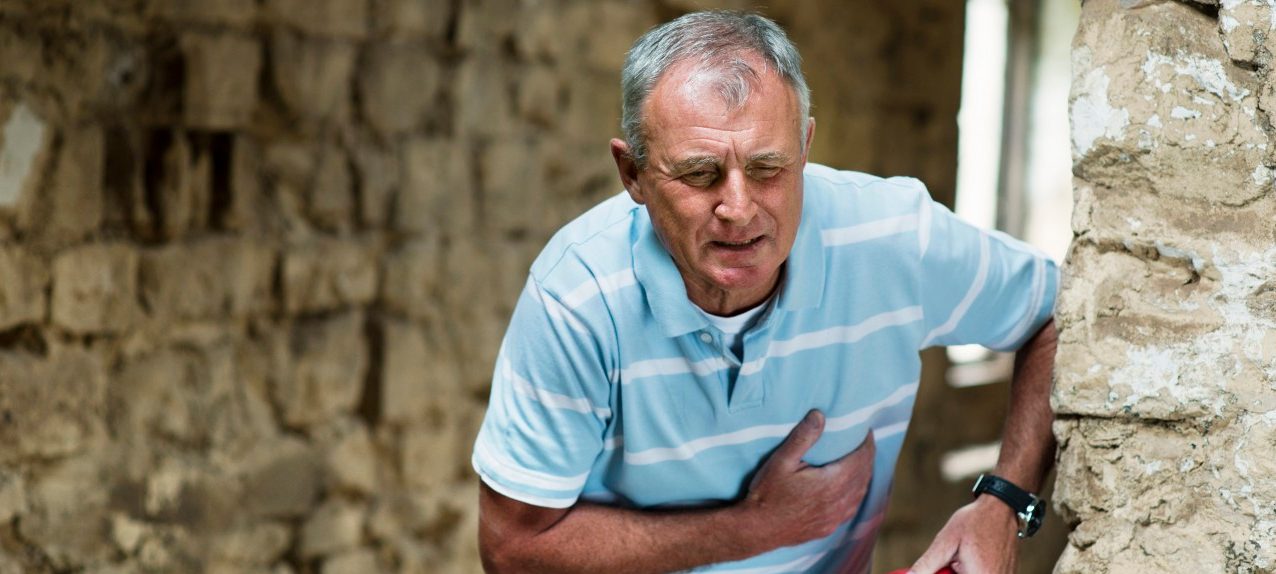
In congestive heart failure, the heart isn’t pumping normally. See your doctor if you have signs of the condition. Early diagnosis and treatment are important.
Almost six million adult Americans have heart failure, according to the Centers for Disease Control and Prevention (CDC). The name of the condition may sound like your heart is going to stop beating — but heart failure simply means your heart isn’t pumping as strongly and normally as it should.
How serious the condition is, and how it impacts life expectancy, depends on many factors, including whether it is diagnosed early, the causes, and treatment.
Heart The terms heart failure and congestive heart failure are often used interchangeably heart failure can start when the left ventricle (one of two large chambers in the heart that collect and pump out blood) becomes stiff or is unable to pump blood forcefully enough to other parts of your body. If the left ventricle fails to move blood adequately, the right side of your heart can lose pumping power, too.
YOU MIGHT ALSO LIKE: Signs and Symptoms of a Blood Clot
Without the heart having enough pumping action to send nutrients and oxygen-rich blood throughout your body, blood can build up in your body. Your kidneys are impacted, too. The result is fluid retention and swelling of legs, ankles, and abdomen. Fluid can also collect in other parts of your body, including the lungs, making breathing difficult.
This is congestive heart failure (CHF), the most serious type of heart failure . It requires diagnosis and treatment as early as possible, according to the American Heart Association. Although the condition is usually not curable, medications, lifestyle changes, and other therapies can help people with CHF improve symptoms.
Are you at risk? Congestive heart failure causes
Any condition that damages and weakens your heart, including a heart attack, can result in CHF, according to the National Heart, Lung and Blood Institute (NHLBI), including:
- Coronary heart disease. A build-up of plaque inside coronary arteries that supply blood to the heart muscle can cause heart disease damage from blood clots and heart attacks. While chest pain is not a specific sign of heart failure, it can be a sign of heart disease which, in turn, may result in CHF.
- Diabetes. Whether you have type 1 or type 2 diabetes, if high blood sugar levels are not well controlled, they can damage and weaken your heart muscle.
- High blood pressure. When blood pressure is consistently too high, over time the pressure not only raises the risk of a heart attack, but high blood pressure can also weaken your heart.
- Thyroid disease. Either too high or too low levels of thyroid hormones, untreated, can lead to CHF.
- Congenital heart defects. Problems with the heart’s structure at birth can result in congestive heart failure in children, unless surgical correction is possible.
- Heart valve disease. You can be born with a defective heart valve, or heart damage resulting from an infection, aging, or other heart conditions can cause heart failure.
You can’t control all causes of CHF, of course, but there are some lifestyle changes that can lower your risk of developing the condition, according to the CDC — including getting regular exercise, avoiding foods high in fat, cholesterol, and sodium, keeping weight at a healthy level, and not smoking.
See your doctor about congestive heart disease symptoms
If you or a family member has these possible symptoms of CHF, the American Heart Association advises talking to your doctor about testing:
- Persistent coughing or wheezing
- Feeling unusually tired
- Edema (excess fluid), especially in your legs, ankles, feet, and abdomen
- Lack of appetite or unexplained nausea
- Thinking difficulties
- Increased heart rate
Bottom line? Getting diagnosed and treated is crucial for heart failure
Diagnosing and treating congestive heart failure as early as possible is the best way to help preserve heart function and quality of life.
Your doctor will diagnose heart failure after studying your medical and family histories, conducting a physical exam, and ordering tests to look for any damage to your heart.
Although no single test can diagnose congestive heart failure, the NHLBI points out, several can help identify the condition.
An EKG to detect and record your heart’s electrical activity, a chest X-ray, echocardiography (to capture a moving picture of your heart), a stress test, and a cardiac MRI to look for heart damage may be ordered. A blood test for thyroid hormone levels and a B-type natriuretic peptide (BNP) blood test, which measures the level of a hormone that rises in heart failure, are also typically part of the work-up for the condition.
Treatment usually involves taking prescription medications, reducing sodium in your diet, managing stress, losing weight, and getting regular exercise. People with CHF also are asked to monitor their symptoms each day so that they can discuss these symptoms with their healthcare team, according to the CDC.
For some people, surgery for heart defects may be appropriate. For patients with severe and late-stage congestive heart failure, implanted left ventricular assist devices (LVADs) can help the weakened heart circulate blood; heart transplants may be an option for certain patients, too.
YOU MIGHT ALSO LIKE: What Is a Brain Natriuretic Peptide (BNP) Test?
Updated:
March 03, 2020
Reviewed By:
Janet O’Dell, RN